Definition and Evaluation of MRI-Based Measures for the Neuroradiological Investigation of Creutzfeld-Jakob Diseases
by Marius George Linguraru and Nicholas Ayache
The identification of diagnosis markers is a major challenge in the clinical care of patients with Creutzfeldt-Jakob Disease (CJD). A study was carried out as part of the French 'GIS-Prions' project to detect and quantify CJD-specific abnormal intensities in Magnetic Resonance Imaging of the brain.
Of great concern has been the occurrence in the United Kingdom in the 1990s of variant CJD (vCJD), a form of human environmentally acquired CJD, also known as 'mad cow disease'. Although the number of vCJD cases has decreased since 2001, a new risk exists of transmission by blood transfusion. The disease raises a number of challenges for neuroradiological centres, since there exists only limited knowledge of how it might be detected through medical imaging. We have studied the detection and quantification of CJD-specific abnormal intensities in magnetic resonance imaging (MRI) of the brain in order to diagnose CJD patients and differentiate vCJD from sporadic CJD (sCJD) cases.
MRI is commonly used for non-invasive examinations of patients with neurological diseases. Some recent studies have found strong correspondences between the diagnosis of CJD and the detection through MRI of signal abnormality in the deep grey matter internal nuclei of the brain. However, observations describing the ability of MRI to assist in the diagnosis of CJD are at an early stage, and the visual interpretation of MR images performed by physicians can be challenging. At present, MRI is not included as a diagnosis criterion for sCJD, but it would be certainly be useful for this and for vCJD. It is therefore necessary to further explore the advantages of Computer Aided Diagnosis (CAD) techniques in the MRI clinical environment.
|
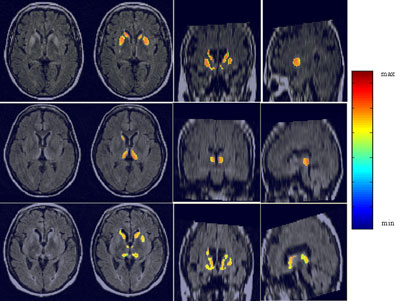
Our method used analysis of deep grey internal nuclei of the brain (namely the head of caudate, putamen and thalamus) to accurately detect human spongiform encephalopathy in multisequence MRI of the brain. T1, T2 and FLAIR-T2 MR sequences were used for the detection of intensity deviations in the internal nuclei. The use of a priori anatomical knowledge in the form of an accurately segmented and labelled atlas facilitated the precise segmentation, while a probabilistic atlas allowed intra- and inter-patient analysis. A feature detection technique based on a model of the human visual system was employed for the depiction of hypersignals. The varieties of human prion disease (sCJD vs vCJD) were differentiated using newly defined MR measures based on the lesions' topographical distribution.
Our database comprised fifteen CJD cases (ten sCJD and five vCJD) and eight healthy controls of the same age range as the patients. All patients showed abnormal intensities in the deep grey nuclei, which were correctly detected by our algorithm. We diagnosed all fifteen prion disease cases with no false positives amongst the controls. The results are robust over the patient data and in accordance with the clinical ground truth.
The caudate nuclei are highlighted as the main area of diagnosis in sCJD, in agreement with the histological data. The algorithm permitted the classification of abnormal signal intensities in sCJD patient FLAIR images with a more significant hypersignal in the caudate nuclei (10/10) and putamen (6/10) than in the thalami. In vCJD patients, we found more significant hyperintensities in the pulvinar than in the other internal nuclei, which confirmed the visually based radiological observations related to CJD. Defining normalized MRI measures of the intensity relations between the internal grey nuclei of patients, we differentiated without ambiguity all CJD cases (sCJD and vCJD) from healthy controls and further classified the CJD patients into two subgroups, sporadic and variant. This is to our knowledge the first attempt towards an automatic classification tool of human spongiform encephalopathies.
The algorithm also allowed the study of asymmetries in CJD MR hypersignals, which has long been a subject of debate by neuropathologists. Using brain internal nuclei masks, we also noted that hypersignals are inhomogeneous over the nuclei.
Our method proved as reliable as the visual interpretation of radiologists for the detection of deep grey internal nuclei hypersignals in MRI of the brain. Moreover, it allowed quantitative data to be automatically obtained from MR patients with CJD, which could be used to follow up patients and evaluate the efficiency of therapeutic procedures. Our study demonstrates the value of MRI as a potential non-invasive diagnostic tool for sCJD and for the characterization of prion diseases.
This work was completed as part of GIS-Prions, a project funded by the French Ministry of Health. The collaboration included the EPIDAURE Research Group at INRIA-Sophia Antipolis, CNRS UPR640-LENA, Paris, the Department of Neuroradiology, La Pitié-Salpêtrière Hospital, Paris, CRMBM UMR CNRS 6612, Marseille, INSERM U360, Paris, and R. Escourolle Neuropathological Laboratory, Paris. The goal was to perform a prospective study of sCJD and vCJD and to develop techniques for the detection and classification of various types of CJD. The database includes CJD patients from two main neuroradiological centres in Paris and Marseille in the period from 2002 to 2004. Contributing members include Miguel Ángel González Ballester, Eric Bardinet, Damien Galanaud, Stéphane Haïk, Baptiste Faucheux, Patrick Cozzone, Didier Dormont and Jean-Philippe Brandel.
Please contact:
Marius George Linguraru, Nicholas Ayache, INRIA, France
Tel: +33 492 38 76 60
E-mail: Marius.Linguraru![]() sophia.inria.fr, Nicholas.Ayache
sophia.inria.fr, Nicholas.Ayache![]() sophia.inria.fr
sophia.inria.fr

 This issue in
This issue in